Practical Placements with SpA: My University Experience Part 2
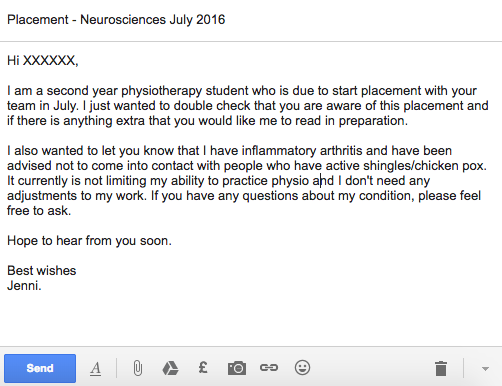
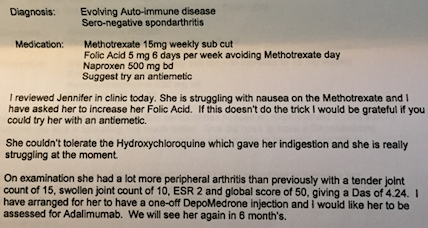
After discussing my previous post ( Studying with Spondyloarthritis ) with a friend over at the National Ankylosing Spondylitis Society's ASone, I have decided to write a follow up post about how I managed my arthritis on placement. Over my three year degree I completed 7 placements that lasted between 2 and 6 weeks (most were 4 or 6 weeks long) in a variety of settings. Over the placements, I was expected to develop my clinical practice and use increasingly advanced and appropriate treatments while under the supervision of a qualified physiotherapist. On placements I could do anything from giving advice, to heavy moving and handling, to facilitating normal movement patterns, to providing walking aids. While some of these were quite light work, others took a lot of effort and most placements involved standing for long periods of time with few breaks. Earlier on in my degree, I really didn't feel comfortable telling my educators that I had arthritis and managed it myself be